|
Tom Frieden Aspen Institute Address on Ebola and Global Health Security delivered 17 November 2014, Washington, D.C.
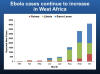
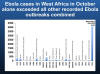
[AUTHENTICITY CERTIFIED: Text version below transcribed directly from audio] Thank you very much for your time. Thanks so much to the Aspen Institute for arranging this, bringing us together. Iím going to go through a fairly large number of slides because I want to get a lot of information out there, but I also want to do two other things. One, leave plenty of time for questions and discussion at the end; and two, remember to leave you with what I think is the single most important concept that Iíll be sharing, and that is that infectious diseases are here to stay but we can make a difference. We can control them and push them back if we focus on three fundamental principles. First, finding threats when they first emerge; second, responding effectively; and third, having learned from those two activities, preventing them wherever possible. And that key formulation of finding, stopping, and preventing is going to be essential to every aspect of our infectious disease control measures. Now, CDC works 24/7 to save lives, protect people, and save money through prevention. We have at CDC more than 12,000 health professionals who work to find, stop, and prevent health threats. We analyze health information in the US and around the world and most of the data that youíll see coming out on health in the US comes from CDC in one way or another. But we also work with individuals, with communities, and with healthcare workers to implement strategies to respond and prevent. We also serve as the de facto reference laboratory for the world, and CDC has more than 200 -- or about 150 different laboratories. We have over 2000 laboratory scientists working on a broad range of areas, infectious diseases, environmental health, bioterrorism, and more. And we have important partnerships all around the world. In fact, CDC has staff in 60 countries. We had staff in Mali before the current cluster and Iíll talk about that more in a moment. We also have a variety of programs that we work around the world with, and again that basic concept of finding, stopping, and preventing is how you can think about our different programs. We have programs in Influenza, so we can track how strains spread around the world, and whatís the best choice for our vaccine here in the US. We have programs in immunization, where we work very closely with the World Health Organization. Measles immunization over the past decade has saved more than 10 million lives and is responsible in and of itself for more than a quarter of all of the increase -- or for all of the decrease in infant mortality or the increase in child survival. Immunization programs are best buys in this country and globally and critically important. We also work on malaria control with the Presidentís Malaria Initiative, and we embed staff into ministries of health where that program is operational. Not dissimilar to what we do in this country where we embed our staff, CDC staff, into State and local health departments. We donít establish large CDC offices all over the country, rather we strengthen the systems in place whether thatís in hospitals -- hospital systems, to support them for better infection control, or public health departments. We do the same thing globally, working with ministries of health and with partners. And of course, the PEPFAR program, which is the largest bilateral global health program there has ever been, and which has been remarkably successful. CDC provides about half of all of the treatment and the prevention of mother to child transmission work in PEPFAR, and in fact, in the Ebola response, the infrastructure established by PEPFAR has been very important in helping to enable us to respond quickly and flexibly. Perhaps the single most important thing we do in global health is a program called the Field Epidemiology Training Program. This is based on the CDC epidemic intelligence service program, a two-year program where you take a highly trained physician or veterinarian or dentist or nurse or pharmacist or Ph.D., and over the next 2 years, you train them to do a very specific style of field epidemiology. You train them to assess the surveillance system and see if itís accurate. You train them to identify and outbreak and stop it. You train them to embed with a local health entity and help them respond to an urgent health threat. That program has been the backbone of the CDC for more than 60 years and now for decades, weíve been helping other countries do a similar type of epidemiology training. And we now have trained over 3,000 epidemiologists from around the world. This is a two-year in-country training program -- 80% of the graduates stay in-country, generally working in positions of leadership. So, this is a suite of programs that allow CDC to strengthen governments, public health systems, healthcare systems around the world for their sake and for ours. And over the past decade, weíve had to respond to a large number of emergencies, natural events, infectious diseases, potential environmental contamination and more. And for the past over two years, weíve been discussing the issue of global health security, because we are truly connected by airplane flights, by food supply, by air, by water, and to a very great extent, our vulnerability depends on how vulnerable other parts of the world are. Now, we have three major risks that we face in global health security. The first are emerging organisms as Ebola emerged in West Africa for the first time ever. The second are resistant organisms and Iíll speak more about that toward the end of this talk, and third, unfortunately, are intentionally created organisms. The same technological advances that allow us to do more faster would allow someone with malicious intent to create organisms that may be difficult to deal with. But we have three opportunities that really give us a lot of hope and momentum here. The first is that there is a public health framework for responding to health security threats. That framework works. Itís committed to by every country. Thereís an evaluation system to assess it, and second, there are real technological advances. So, now weíre able to do rapid testing for example for the plague bacteria in just 20 minutes with a dipstick that looks like a urine test or a pregnancy dipstick. That test is in clinical trials in Africa today, and has already been used to rapidly detect and as a result, able to treat and prevent outbreaks from plagues. So, there are technological improvements, not just in laboratory work but also in informatics and in communications technologies. And third, there are success stories, whether itís Chinaís successful containment of H7N9, very different from what happened with SARS a decade earlier or Thailandís setting up a system by which they can track and stop flu or the global collaboration in response to a variety of threats. We have successes, and that leads us to the goal of prevention, detection, and response. The global air network is quite striking and we are ever more connected. Interestingly, West Africa is closer to Europe than it is to East Africa or Southern Africa, but I think in many quarters, thereís a little bit of a conflation of what is Africa, what is West Africa. The West African countries that have been heavily affected by Ebola are struggling and beginning to show proof of principle that we can stop it, but we have a long way to go there. Global health security is something that weíve committed to for several years. We implemented pilot programs in 2013. Those pilot programs showed real success and promise and one in Uganda for example was able to result in very rapid detection of outbreaks of meningitis, cholera, of Marburg virus and allow very rapid response. Our goal in 2014 has been to implement together with the Department of Defense in 10 countries programs to advance this prevention detection response framework. In 2015, weíre hopeful that with the emergency request of the president, weíre able to really begin to close some of the blind spots to address some of the weak links that make vulnerabilities around the world our vulnerabilities. And the commitment is that by 2020, we will have 30 countries with at least 4 million people effectively prevented -- protected against another outbreak. The approach is very straightforward. Itís again that prevention detection response framework. In prevention, we start with biosecurity and biosafety, making sure that laboratories are safe, so that organisms donít unintentionally or intentionally get out and infect laboratory workers and escape to the community. Immunization programs, which are a tremendously effective way not only of promoting health but of reducing health risks that may spread more broadly, and nothing could make that more apparent than what weíve been dealing with with measles over the past couple of years where outbreaks anywhere in the world results often in outbreaks here. Measles is very highly infectious. We also are focusing on surveillance for zoonotic disease in humans. About three-quarters of all newly emerging infections come from some part of the zoonotic world, some part of the animal kingdom, and we still do not have a handle on the natural reservoir of Ebola, but studies are underway now, so we can understand that better and prevent future events where Ebola would be introduced into a society. On the prevention front, there is also antimicrobial resistance prevention, and that means both antibiotic stewardship which Iíll talk more about, but also identifying and stopping the spread of resistant organisms. On detection, critically important that we monitor to detect threats early. What a different world we would be in today if these basic systems had been in place in West Africa a year ago. It doesnít take much to identify a cluster of people with hemorrhagic illness. Itís a very unusual disease. It doesnít take that much to do laboratory testing for it. It does take a lot to stop it even if itís very small. And it takes an enormous amount to stop it if itís become epidemic which is what happened -- what has happened now. But that means having information systems, that means having disease detectives, people whoíve been through training like the field epidemiology training course I mentioned, and then response capacity. And response capacity means having an incident management system with an emergency operation center. This is fundamentally how we organize to respond to an emergency and for the global health security work, we have the metric -- key metric that every country and every subnationality within countries should be able to activate their emergency operation center and respond within 2 hours to a threat. If you can do that, you can cut the time out of steps and you can respond much more effectively and prevent things from getting as out of control as the Ebola has gotten now. Now, to talk about Ebola for a minute. We look at different infectious disease threats and Ebola is scary. Itís scary because of its case fatality rate, which is generally in the 50-70% range. We think that with meticulous clinical care, we should be able to get that down substantially, addressing hydration and fluid management, but itís still a very deadly disease. Compare that with things like SARS, which is around 10% or MERS which is as far as we know is about third -- or even the 1918 pandemic, which was about 2%, 1-2% in those who it infected. The case fatality rate as we call it in public health is high. But that doesnít mean that it has anything like the epidemic potential of influenza, because one of the fundamental facts about Ebola is that from everything we have seen, it only spreads from someone who is ill and it only spreads from direct contact with body fluids of someone who is ill or someone who has died. So, the spread has been primarily by these two routes, unsafe caregiving whether in the home or in healthcare facilities and in Africa, unsafe burials, where burial practices and way may promote the widespread transmission of disease. Now, the bottom line with Ebola is that despite recent progress, the epidemic remains severe, that core public health interventions can stop it, and that success requires speed and scale deploying effective prevention and control resources. Now, I think there are three overarching principles that are essential to the response. The first is speed; the second is flexibility; and the third is keeping the front lines first. Just to mention speed for a moment, models constructed by CDC epidemiologist indicated that even a 1-month delay in scaling up services to respond to Ebola could result in a crippling of the size of the outbreak, and thatís why weíve been working around the clock for the past 4-6 months and thatís why weíve been working around the clock for the past three days surging people into Mali to deal with the cluster there, which Iíll talk about more in a minute. Flexibility is very important. The incubation time of Ebola is 2-21 days but the usual incubation time is about 8-10 days. That means that every week and a half thereís another generation of cases and youíve got to be ready to respond wherever itís most needed. The front lines first is a key concept. Staff who are working in West Africa continue to be frustrated by the lack of simple things that would be very helpful in response. CDC has 170 staff on the ground now in West Africa. It is the largest global response in our history, and weíve been aided enormously by our partnership with the DOD, with USAID, and their DART process, or Disaster Assistance Response Team process, but despite all of the good wishes, still we deal with things like the need to get into a village thatís so remote that not even helicopters can get us there or to take dugout canoes to get to a place where thereís a cluster of cases or to hike 4 hours through a forested area to get to a diamond mine where we find not just a cluster or Ebola but 20,000 people living and working around that diamond mine and where if we donít get in and get specimens out, we may have a cluster of hundreds or even thousands of cases. So, those are the three key principles that we try to ensure adherence to. The way to think about the Ebola outbreak I think is as a forest fire or analogous to a forest fire. At the center are Liberia, Sierra Leone, and Guinea, which have in various different parts of their country, bush fires all over, widespread -- the first time the world has ever had an epidemic of Ebola spreading widely throughout countries, spreading to multiple countries. But around them, are the sparks that emerge from that forest fire, and that might land in Lagos, Nigeria, or Bamako, Mali or Senegal. And each of those sparks has the potential to create another set of wild fires, another forest fire unless itís rapidly extinguished by intensive effort, and just to give you a sense of how intensive that effort needs to be, in Nigeria, when an ill traveler went from Liberia to Lagos, and was so ill he had to be carried off the plane, he went to a local hospital, his Ebola diagnosis was initially not suspected, and pretty soon, there was a cluster of cases in Lagos. At CDC, we had staff on the ground who were working on polio eradication in Nigeria as well as the PEPFAR program and Malaria work, we could bring staff from other parts of Africa and within 48 hours, we put 10 of our top staff on the ground in Lagos. We were able to help the government repurpose their polio infrastructure to manage the Lagos outbreak. We were able to take 40 of the trainees that we had helped become disease detectives to deal with polio, Nigerian doctors, and reallocate their work to Ebola control. And over the following weeks, they identified 899 contacts. They did 19,000 home visits to monitor for fever. They constructed an Ebola treatment unit. They trained more than 2,000 healthcare workers in Ebola prevention and control. They got more than 95% of their contacts monitored every day. They missed one. That one contact went to another city called Port Harcourt and started another cluster of Ebola there. That they repeat the operation there, creating an emergency operation center, training staff, creating treatment facilities, but with all that intensive work, they were able to stop the outbreak, and from that importation event, Nigeria is now Ebola free. Thatís the effort it took to prevent one case of Ebola from becoming an outbreak or epidemic and even how central Nigeria is to African travel and transit, it was crucial to do that. Thatís the struggle we are today engaged in in Mali. And then beyond that second ring of countries that may have an immediate ember or spark that ignites an outbreak, every other country that has the potential to have Ebola or other deadly infectious diseases needs to become more fire resistant. And fire resistance in the case of infectious disease control means detection systems -- you find things early; response systems, so you can respond effectively; and prevention. Those same three principles. In Ebola control, we have five basic principles: [1] Incident management, organizing our system so that itís efficient. Last week, we ensured that Mali had appointed an incident manager and we are now scaffolding around that individual to provide as effective incident management as possible; [2] Treatment in Mali, the government of Mali had created an Ebola treatment unit to provide isolation and care, and now they have one confirmed and two suspected patients in that Ebola treatment unit which is currently being staffed by Doctors without Borders from Spain, MSF Spain; [3] Burial support, and in parts of Africa, burial traditions are very different from here and involved washing the body, touching the body, sometimes whole villages touching bodies to pay respect. Itís their way of grieving. It needs to change to protect people from Ebola, but that means change in communities that are very widely dispersed, which donít have a lot of trust often of the government and society, which may be cut off without internet, cellphone, even radio coverage with the rest of the world. So, this is a challenge; [4] Fourth is infection control in the entire healthcare system. We have to ensure that the whole healthcare system in these three West African countries is ready to consider Ebola and thatís not easy. Because it initially prevents -- presents quite a bit like malaria, and these are countries that are hyperendemic for malaria. The rate of malaria infection in these countries is in the range of 20, 40, 50, 60, even 70% in different communities. So where you have something thatís very common and looks a lot like something thatís a lot less common but a lot more deadly to the healthcare workers, you have to have an overarching change in the way infection control is done; [5] And finally, communication to get all of these through to healthcare workers and to the public. CDC has as I mentioned the largest global response in our history and is addressing all aspects of the response in conjunction with our US and global partners. That includes addressing the needs in each of the countries and though the -- many of the US efforts are focused on Liberia, the CDC efforts are acting in every country where there are cases. We actually have more staff in Sierra Leone than in Liberia because the needs are greater there at the moment. In Sierra Leone, the British government has come in in a big way with assistance and working very closely with the UK to provide the kind of information and feedback and guidance and partnership that is most effective, but everything from laboratory testing to communications expertise, to contact tracing, to outbreak control, to logistics, are things that CDC along with USAID, WHO, and others and the Department of Defense, which has come in in a very big way, in a very helpful way are doing. Now, there has been -- there have been some encouraging trends in some parts of each of the three countries, and I believe those encouraging trends are fundamentally proof of principle that we can still stop Ebola; but Iíve heard at times some sense of the problem is over already, and Iím very concerned by that perspective because itís nowhere near over. Itís going to be a very long, hard fight because every single one of those cases thatís emerging and theyíre now many hundreds, probably more than a thousand cases a week emerging in West Africa. Every one of those cases needs that kind of response that I described for Lagos, Nigeria. And that is going to be incredibly difficult. So, we have a long way to go and just to give you a sense of how far weíd have to go, a reminder that cases are still growing. Despite some progress, there are more cases in West Africa in October than there were in September and though the number is decreased somewhat in Liberia, we believe thereís still so many cases that weíre not able to do the kind of outbreak control thatís needed and there are so many communities that have not yet had cases that needed intensive control measures. In fact, in October, West Africa had more Ebola cases than in all other recorded Ebola outbreaks over the last 40 years combined. So, we have a long way to go, but we do have proof of principle, and we do have tremendous commitment from societies. My team in Liberia was describing how many communities themselves were taking action. Their remote services havenít gotten there, so they identified buildings or schools to isolate and care for people with Ebola. They track the contacts so that they would be rapidly isolated and wouldnít further spread disease. So, thereís a lot of progress. I did want to share with you -- this is actually outdated because itís from yesterday. I had updated slides from this morning, but we didnít have a chance to put it in yet. One additional case has been confirmed and this is just an example of the kind of rapid assessment that weíre doing for the Malian cluster. One individual, a 70-year-old man, the Grand Imam of Kouremale became ill and died. It was not understood that he had Ebola, and in all likelihood he did. In all likelihood, he may have gotten it by performing some of those funeral rites that were mentioned, but he was the Grand Imam of a large town that is literally on the border between Guinea and Mali. Somebody said to me, you mean like Kansas City. I said, well, yeah, kind of, but not in a lot of other ways. But it is a town that straddles two countries and when he became ill, he had other conditions. He was taken to three different healthcare facilities, and then he had a large funeral service, and in those healthcare facilities, he was cared for by his family and he was cared for by individuals who have since been confirmed to have had Ebola. The team there has now identified more than 450 contacts and theyíve undertaken contact tracing to track those individuals ideally every day for 21 days, so that the moment anyone gets sick, they get isolated. We expect people to get sick because thereís flu, thereís malaria, thereís typhoid, thereís other febrile conditions and an indicator of this system working is that people would be brought in to the Ebola treatment unit and tested. We already had two, tested negative. When you have a negative test, you have to repeat it 72 hours after symptom onset because early on, thereís so little virus that the individual is not infectious but they also canít be diagnosed in some cases. This is just a map of what happened. You can see on the border, Kouremale and then they travel to -- to Bamako. One of the things that we do is to help countries establish exit screening, so that every person who leaves is screened. Their temperature is taken. They are asked a series of questions and in this process, over the past few months, weíve identified more than 80 people whoíve had fever and theyíve not flown because they had fever. In many cases, they actually didnít even enter the airport because the screening is done at the airport entrance, and that temperature is often retaken several times by the airlines or others as a way of keeping febrile people off airplanes. Now, we also have looked at that second and third ring of preparedness. And this is a slide created I believe before the Malian cluster. And you could kind of see that thereís roughly speaking some green. Weíve got laboratory capacity in most of the countries. Some of them, itís challenging. But thereís a whole lot of red, emergency response capacity and thereís even more yellow, where weíre not there yet, and thatís why the emergency funding request is so critically important, because today or yesterday or tomorrow, there could be another exposure, likely exposure in Mali, and weíll be dealing with another potential outbreak. And every one of these countries has the risk of either being like Lagos and controlling that spark or like the next Liberia or Sierra Leone, with widespread transmission throughout the society and that kind of widespread transmission doesnít just harm people from Ebola, it really cripples the healthcare system. The healthcare system is basically closed. People donít come in for vaccines, they donít come in for treatment of malaria. Women who need emergency obstetrical care donít come forward for it. People who have car crashes and are bleeding are not cared for in some circumstances because people are afraid it might be Ebola. And the effect on society more generally are also devastating. Schools are closed. The economies are suffering severely. Crops are either not being planted or harvested to the extent that it could be otherwise. So, the Ebola epidemic in West Africa has impact far beyond Ebola and far beyond the health system. But thereís also progress. This is a women I met in Liberia. She lives on the Firestone rubber plantation. Firestone had a cluster of Ebola. They went to the government and said help us. The government said we canít -- weíre too busy. So, the Firestone people said okay, where can we learn how to do it ourselves? They said you better talk to MSF Doctors without Borders. They did. They created their own Ebola treatment unit. They monitored every one of their contacts, and they were able to stop the spread of Ebola for their population of 55,000 people living on the largest rubber plantation in the world. And this is one of the survivors of that effort. So, in the US, there are a series of things that weíre doing to strengthen our preparedness against Ebola, screening and monitoring of travelers when they leave affected countries and when they arrive in the US. When they arrive in the US, their temperature is taken again; detailed information is taken about their contacts, so that local and state health departments can monitor them for 21 days in case they become ill, and theyíre provided with a care package, Check and Report Ebola, and that care package has a thermometer, a fever log, health information, a wallet card, a number to call if they get sick. And over the past couple of weeks, at least 4 people have gotten sick. Theyíve taken their temperature. Theyíve had a fever. Theyíve called that number. The State Health Department has arranged for safe transport of the individual from where there are to a hospital thatís ready and waiting for them, and all four of them ruled out for Ebola, but they were called for safely in that system. Yesterday, we notified people that starting today, weíll be doing that same kind of active monitoring for everyone arriving from Mali, not because we believe thereís widespread transmission in Mali today but because there are so many contacts there and weíre not yet confident that those contacts are all being identified and monitored daily. So if one comes here, we donít want to take the risk that they might become ill and then the healthcare system would not be aware of their illness in time. We donít know that we have the perfect response, but like everything in public health, everything in clinical medicine, everything in science, we use data to continuously improve practices. Thatís the approach we take and thatís the approach weíll continue to take. Weíve also worked with the healthcare system to strengthen infection control, to think Ebola earlier, to provide assistance in the form of what are called REP teams, or Rapid Ebola Preparedness teams, which have now visited more than three dozen hospitals all over the country in a dozen states -- to assess whether they are ready to care for an Ebola patient; to make sure that they are linked up with a laboratory. Weíve now got more than 30 laboratories around the country that CDC has trained and supplied with partnership from DOD which had provided the assays so that they can do tests for Ebola. It used to be only CDC and USAMRIID could do test in the US, not we have more than 30 laboratories that can in the public health system. And the REP team will look very closely at whether the hospital is ready and what more they need to do to get ready. Now, in the emergency budget request, the funds requested are divided into on the one hand immediate and on the other hand, contingency. The immediate request is divided into three parts: domestic, Ebola, and a broader global health security component. For the CDC aspects of that request, itís a request of 1.83 billion dollars divided almost equally between those three components of domestic preparedness, Ebola specific work in West Africa, and global health security work. This is absolutely critical. We have currently 30 million dollars stop gap funding that expires on December 11th. That money is all committed. It allowed us to keep going at the level at which weíre going but not to scale up and ramp up to do the kind of outbreak control needed or to stop and make all those yellow and red boxes green for the surrounding countries. If we donít do that, we canít with confidence say that weíll be able to make the next outbreak the next Lagos and not the next Liberia. Now, global health security is something weíve been working on for some time, and that whole framework of prevention, detect, and response has clear parallels with the Ebola work. In fact, thereís tremendous synergy between preparing for Ebola and preparing for other health threats, and I think it would be irresponsible of us with scarce dollars not to ensure that we stretch them as far as possible so that weíre addressing Ebola but also if we happen to get lots of fever next time, we havenít not prepared -- weíre prepared for that as well. So the approach really is prevention through, in the case of Ebola, things like infection control, biosafety more broadly. In terms of detection, laboratory disease surveillance and a trained work force who can find the Ebola or the next health threat that may be unexpected from an unexpected part of the world, and to respond effectively. Now, I want to before closing just talk about a little bit more than just Ebola because the Ebola has been pretty all consuming for many of us for a long time. Thereís a lot else going on. In 2014, Congress approved our top priority act at CDC and that was something called Advanced Molecular Detection -- funding to do something thatís quite exciting: to be able to go into what itís called sometimes -- Next-generation sequencing. Next-generation sequencing: Instead of growing up an organism in the laboratory and then analyzing its genetic code, we actually take the sample itself, sputum or blood or other clinical specimen and we look into that sample to understand in a much different way, a much deeper way, whatís actually happening with that infection. And we donít know whatís going to come out of this. We think we can get more rapid diagnostics of infections, of drug resistance, perhaps identify what are the strains that are spreading more. It may change the way we understand certain infections. There may be co-infections of multiple organisms or the substrain that grows really well in the laboratory may not actually be the strain thatís making someone the sickest when we get that actual specimen data. So, thatís all interesting theoretically but what does it mean practically? It means that we can save lives; we can save money; and we can save time. We can cut time out of outbreak detection and response and make outbreaks smaller. Thatís the promise but we need to continue to invest in it, work hard, and work smart. I had the pleasure of walking through a poster session at CDC where we had dozens of laboratories and epidemiologic groups around CDC thinking through how to apply this to their work. Perhaps there are cases that were considered to be unrelated but actually are part of a cluster or in another disease. Thereís something that we assume there was one outbreak and it turns out it was multiple different outbreaks, each of which had different sources and needed different interventions. So, this is a very exciting new way of combining traditional epidemiology with genetic sequencing, bioinformatics that needs to be incredibly powerful to achieve this advanced molecular detection. Even one of our rapid sequencing machines in one two-hour run can create enough data to overload 100 computers. So, the amount of data thatís coming out of it and the need to analyze that thoughtfully is -- is mindboggling. We think that over the five years of this initiative weíll transform the way we do genetic epidemiology and epidemiologic investigations for some of our conditions, be able to identify things sooner, finding diagnostics that can make a diagnosis in a shorter period of time, helping states implementing sustainable systems and developing more predictive modeling measures. New technologies donít take the place of careful analytic work. They may point in a direction where we can be more fruitful in our analytic work, but they donít take the place of that really thoughtful complicated work, and fundamentally, that will lead to better detection, and better surveillance. Now, one of the things that we need to look at closely is antimicrobial resistance. In the US and globally, weíre seeing an inexorable rise in drug resistance -- faster for some organisms, faster in some parts of the world. And last year for the first time, CDC did an overarching report on drug resistance. We identified that there were more than two million drug resistant infections in the US each year, even conservatively estimated, and more than 23,000 deaths. In addition, there were 14,000 people who died related to C. difficile, which is a complication of antibiotic use. So, this is a serious health problem. As an infectious disease physician myself, Iíve treated patients for whom there are no modern medicines. Itís a horrible and helpless feeling for physicians, for patients, and for families. And it reflects the fact that for some patients and some organisms, weíre not in the pre-antibiotic era, weíre not in the antibiotic era, weíre in a post-antibiotic era; and unless we take urgent action, a greater proportion of infections will be difficult if not impossible to treat with modern medicines. And itís not just about treatment of infections because routine infections like pneumonia, urinary tract infections might become very difficult to treat. Weíre tracking one particular organism called CRE or Carbapenem-Resistant Enterobacteriaceae and that organism can be resistant to all antibiotics and currently itís mostly in hospitals. But if it spreads out to the community, then routine urinary tract infections may become extremely difficult to treat. But itís not only the infections themselves. Treatment of infection has become an integral part of modern medical care. Whether thatís cancer chemotherapy, transplant, treatment of arthritis, joint replacement, complex surgery, dialysis, all of these things depend on the ability to rescue patients when their immune system is low with effective antibiotics. In fact, more than 600,000 Americans will get cancer chemotherapy this year. About 60,000 of them will be infected -- will be hospitalized with a serious infection thatís a complication of their chemotherapy, and 1-in-14 of those may die from that complication. The more resistant organisms we get, the higher that proportion, the greater the risk of cancer treatment. Thatís just one example and weíve identified seven particular threats. I mentioned C. difficile. I mentioned CRE. There are others as well. We think that we can actually substantially reduce the burden of these risks. In fact, youíll see this looks quite familiar to what I said earlier, detection, response prevention, and also innovation for new diagnostics and new treatments. We have a proposal in FY15 to accelerate the detection and response to drug-resistant infections and to improve infection prevention and antibiotic prescribing. We think that between about a third and a half of antibiotic use in this country are either unnecessary in the first place or are inappropriately broad-spectrum. So, we have a long way to go to improve our own prescribing practices. And we can begin to address the gaps that can reverse drug-resistance. In fact, we think we can make significant progress. We think we can cut C. diff and CRE by 50% over a five-year period -- and thatís not just a guess. Thatís what the best performing systems have already done. Thatís what other countries have already done. And we know how to do it. What we donít have are the resources to do it at scale. In fact, we estimate that if we have this kind of multi-sectoral intervention, over five years we can prevent over 600,000 multi-drug resistant infections, and over 37,000 deaths, and save nearly 8 billion dollars in healthcare cost. These are two lines: one, if we keep going as weíve already gone; the other, if we implement intensively and aggressively. Antibiotic stewardship is one of the key areas. It requires commitment, leadership, tracking. We now recommend that every hospital in America have an antimicrobial stewardship program. We think it has tremendous benefits for the facilities. It also is a win-win. It saves money and it saves lives. The National Healthcare Safety Network operated by CDC now includes virtually every hospital in the country -- plus dialysis facilities and outpatient surgical facilities. An increasing number of facilities report electronically and weíve had a very productive collaboration with the Center for Medicare and Medicaid Services to use this information to feedback to hospitals and payers and encourage rapid progress. But antimicrobial resistance is a time bomb, and weíve got to stop it before it gets too late, before the routine infections that we all could get tomorrow are not easily treatable. Weíve got to preserve the antibiotics and weíve been using for our kids and our grandkids because the pipeline is not full of new drugs about to come out. We hope new drugs will come out but unless we improve systems of using the antibiotic agents today, we could lose those as quickly as weíve lost these. Page Updated: 5/31/20 U.S Copyright Status: Text & Slides = Public domain. |
|
|
© Copyright 2001-Present. |